Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Pride Publishing Inc.
All Rights reserved
All Rights reserved
Scroll To Top










By continuing to use our site, you agree to our Private Policy and Terms of Use.
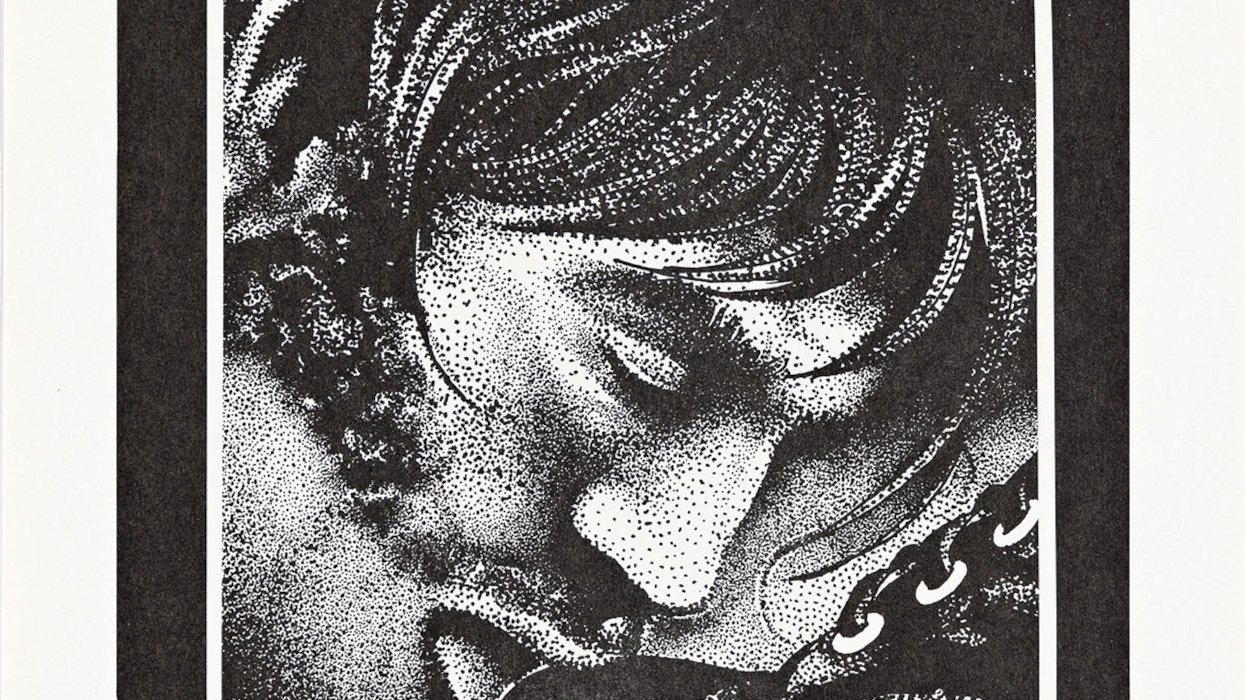
30 Things (Number 1-3)
1. I just tested positive for HIV. Could it be a mistake? Although false-positives aren’t common you should have a confirmatory test, basically a second test to verify your results. The likelihood of two false positives is extremely rare. If you took the at-home test, it’s a good idea to have a doctor or clinic run the second test.
2. My partner’s test was negative, are they in the clear? Unfortunately, false-negative test results can happen too, so if your partner gets negative results and yours came back positive, it is wise to be cautious and have your partner retested. According to AIDS.gov, the likelihood of a false negative depends on the time between when you might have been exposed to HIV and when you take the test: “It takes time for seroconversion to occur. This is when your body begins to produce the antibodies an HIV test is looking for—anywhere from two weeks to six months after infection. So if you have an HIV test with a negative result within three months of your last possible exposure to HIV, the Centers for Disease Control and Prevention recommends that you be retested three months after that first screening test. A negative result is only accurate if you haven’t had any risks for HIV infection in the last six months—and a negative result is only good for past exposure.”
3. How did I get HIV? This is a question you’ll ask and get asked exhaustively, and the bottom line is that you likely acquired the HIV virus by coming in contact with the blood or semen of someone who is HIV positive. The most common modes of transmission include unprotected anal or vaginal sex and sharing needles (regardless of whether they are for injecting drugs or medication like gender-confirming hormones). The CDC says it’s still possible to also acquire HIV through contact with blood, blood transfusions, blood products, or organ transplantation, “though this risk is extremely remote due to rigorous testing of the U.S. blood supply and donated organs.”










 Replay Gallery
Replay Gallery