The data supporting the use of Truvada as pre-exposure prophylaxis (PrEP) continues to build, with another European study
halted this week due to high efficacy rates.
A French study of gay men at risk for HIV infection, known as IPERGAY, was closed due to high success rates so that Truvada could be made available to all 400 trial participants. Half of those participating had been taking a placedo.
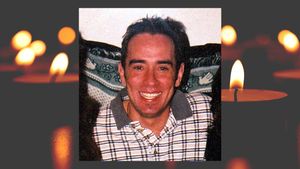
While complete results of IPERGAY will not be available until early 2015, trials are typically halted if high efficacy rates are acheived earlier in the process. Professor Jean-Francois Delfraissy, director of the French National AIDS Research Institute (pictured), called the their early results "a significant breakthrough in the fight against HIV and AIDS."
Even more intriguing was the IPERGAY regimen design. Rather than the one-pill-a-day dosing used in previous trials, subjects were given a "PrEP on demand" dosage schedule. The regimen calls for two pills at least two hours prior to sexual activity, and then one pill for each of the next two days. Previous trials have also shown efficacy with as few as four pills per week, but the "Prep on demand" model appears to focus the
medication around actual sexual activity, when the body may need it most. (See graphic below.)

Only two weeks ago, a British study known as PROUD
was also ceased because efficacy surpassed what was originally anticipated by researchers. Participants there who had been taking a placebo were called back to clinics and offered Truvada. Presently, the United States is the only country in which Truvada has been approved for the purposes of pre-exposure prophylaxis, although that is likely to change in light of the these new study results.
"These studies demolish several assertions made by critics of PrEP," said Gus Cairns of
AIDSMap. "Firstly, that condoms work better than PrEP. They don't. Secondly, that people won't adhere to PrEP. They will. And thirdly, that there will be a public health disaster if people switch condoms for PrEP. There won't be. Condoms will remain an important part of HIV prevention and probably the method used by the majority of gay men for some time to come and there will always be men who prefer rubber to pills, as there are women to the contraceptive pill."
Cairns believes that while the evidence for the use of PrEP is reaching critical mass, even more options for HIV prevention must be sought and studied. This year may have the same historical impact as 1996, the year combination therapy emerged, he said.
"We need more," said Cairns. "We need a microbicide lube we can add to this. We need similar prophylaxis for STIs. We need a vaccine. We'll get them in the end, and eventually the days when the only thing we had to protect ourselves from HIV was a piece of rubber will recede into the past."