By Catherine Tang
In 2008, a Black man from Louisiana was charged with a felony for intentional “exposure to AIDS,” despite not having it. Instead, the man was diagnosed with HIV and had been receiving consistent medical care since. In 2010, an HIV-positive protester in Maryland was given five years in prison for second-degree assault because he spit on a police officer. From 2008 to 2013, at least 180 people living with HIV (PLHIV) were arrested or charged under HIV criminalization laws.
During the early years of the epidemic, public fear and a widespread stigma against HIV incited a global rush to prosecute HIV-positive individuals. The U.S. became the first country to introduce HIV-specific criminal laws in 1987, establishing penalties for “failing to disclose infection, for exposing others to the disease, and for transmitting the disease intentionally or unintentionally,” according to American Academy of HIV Medicine. The passage of the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act in 1990 required states to prove they had laws in place to prosecute HIV-infected individuals who knowingly exposed others to HIV — and currently, 35 states have varying degrees of HIV criminalization laws, according to the Centers for Disease Control.
 Photo by McGregor LightRocket via Getty Images
Photo by McGregor LightRocket via Getty Images
On the surface, laws requiring the disclosure of one’s HIV status before participating in activities that increase transmission risk may seem like a good idea. Yet a 2016 study revealed that in the states that had HIV criminalization statutes, there was no correlation between the laws and HIV diagnoses. Additionally, the majority of such laws were passed before medication mitigating or preventing HIV was even developed. For example, antiretroviral therapy can virally suppress HIV and prevent individuals from transmitting the virus to others. Pre-exposure prophylaxis (PrEP) can reduce the risk of HIV transmission by 99 percent. However, HIV criminalization laws continue to apply, despite any protective measures PLHIV may take.
Yet, most HIV-specific laws are not applied to other sexually transmitted diseases such as hepatitis C and B. As a result, laws often impose criminal liability solely on the basis that the defendant was HIV-positive, meaning some were prosecuted despite a lack of actual transmission or in cases where the risk of transmission was very low. For instance, several states criminalize biting, spitting, or oral sex by HIV-positive persons, yet saliva is not a scientifically proven transmission risk. Widespread ignorance and stigma have also caused PLHIV’s blood, semen, and saliva to even sometimes be referred to as “deadly weapons,” meaning they could be charged with aggravated assault, attempted murder, and even bioterrorism. Consequently, HIV exposure laws could very well backfire. For example, fear of criminalization could dissuade PLHIV from discussing their sexual behavior with doctors because doctors’ notes could later be subpoenaed, and the laws could also prompt people at risk not to get tested because knowing their HIV status would make them legally culpable. In other words, someone who is HIV-positive but does not know their status cannot be prosecuted. Yet, if someone decides to get tested and finds out that they are HIV-positive, they can then be prosecuted.
HIV criminalization laws also disproportionately impact historically marginalized groups, including people of color, sex workers, and men who have sex with other men (MSM). As a virus that is extremely vulnerable to factors like poverty and stigma, HIV is especially prevalent in under-resourced neighborhoods that face a variety of barriers to HIV care and prevention. Chief among them is housing instability, with PLHIV making up 3.3 percent of the homeless population in 2010, and the rates of HIV are much higher among those who experience homelessness than among the general population. Racial minorities who reside in less affluent neighborhoods also have more interactions with the police, making them more susceptible to becoming targets of HIV-related crimes; Black men are much more likely to be convicted of HIV-related crimes than white men, according to the Williams Institute. Sex workers are also another group disproportionately harmed. For instance, among the 800 cases of prosecutions under HIV-related laws in California between 1998 and 2014, 95 percent involved sex workers or people accused of sex work. Compounding excessive criminalization, many PLHIV are unaware that such laws even exist. A 2017 study revealed that across 16 states, 75 percent of MSM, whether HIV-positive or not, were unaware of their state laws, making them even more vulnerable to incarceration. The study also showed that, among PLHIV who were aware of their state’s HIV criminalization laws, that knowledge did little to change their behavior when it came to condomless anal sex.
 California Congresswoman Barbara Lee (photo by Leigh Vogel/Getty Images)
California Congresswoman Barbara Lee (photo by Leigh Vogel/Getty Images)
Currently, there are no federal laws explicitly addressing HIV criminalization, although several laws have been introduced but failed in committee. One of them is the Repeal Existing Policies that Encourage and Allow Legal (REPEAL) HIV Discrimination Act, which was introduced in 2013 by Congresswoman Barbara Lee, a California Democrat. While a number of its recommendations have been adopted by numerous state and federal agencies and initiatives, such as the National AIDS Strategy, the CDC, the Department of Justice, and the Uniform Code of Military Justice, the legislation has yet to achieve congressional approval from the House or Senate.
Recent years have seen pushback from activists and legislators to repeal or modernize outdated HIV criminalization laws at the state level. Texas repealed its criminalization statutes in 1994, yet PLHIV can still be prosecuted under general criminal laws and face charges such as attempted murder and aggravated assault. In July 2021, Illinois’s House Bill 1063 repealed the Illinois Criminal Transmission of HIV statute, which eliminated the threat of prosecution and incarceration for PLHIV and instead treated HIV as any other long-term chronic disease.
Since 2014, 11 additional states, including California, Michigan, Missouri, Nevada, and North Carolina, have modernized their laws. These enacted measures include requiring proof of intent to transmit, taking into account PLHIV who took practical measures to prevent HIV transmission (such as antiretroviral and condom use), reducing criminalization penalties from a felony to a misdemeanor, and removing the provision from the criminal code to be part of the administrative code as a measure to help control communicable diseases. It is important to note, however, that there are reasons to remain cautious despite significant progress. For instance, modernized laws preventing prosecution of PLHIV who are virally suppressed may exclude groups, such as sex workers, who are already less likely to access the services they need to achieve an undetectable viral load.
HIV decriminalization necessitates a multifaceted re-examination and redefinition of legislation and societal structures, which can’t be solved by a silver bullet solution. Rather, laws should be written intending to not only prevent transmission but also to protect PLHIV, and scientific advancements necessitate legal modernization as new therapies and treatments continue to greatly reduce transmission risk. Ultimately, people living with HIV should not be prosecuted simply because the law cannot keep pace with science.
The author of this article, Catherine Tang, is a freshman at the University of Pennsylvania majoring in Health and Societies with a concentration in Health Policy & Law.
From Your Site Articles
Related Articles Around the Web
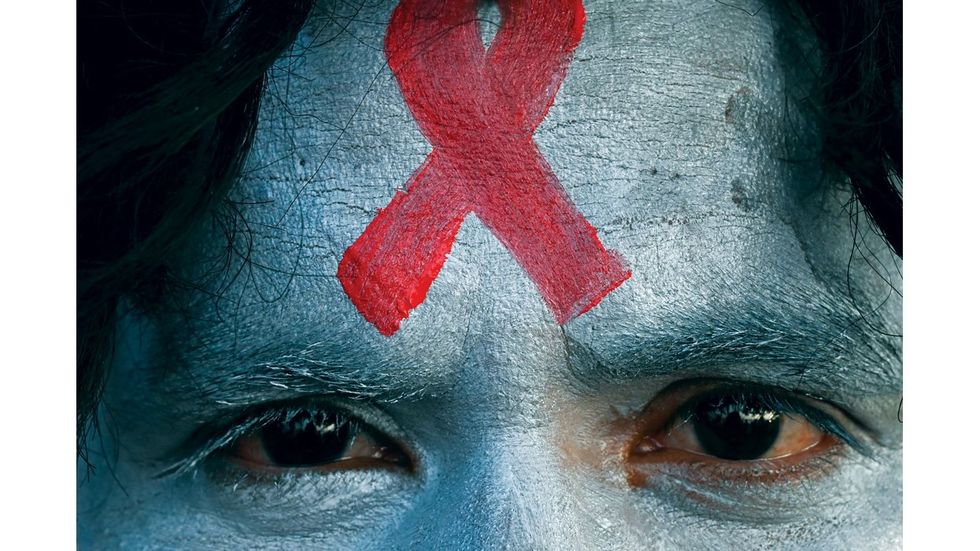
 Photo by McGregor LightRocket via Getty Images
Photo by McGregor LightRocket via Getty Images





























 California Congresswoman Barbara Lee (photo by Leigh Vogel/Getty Images)
California Congresswoman Barbara Lee (photo by Leigh Vogel/Getty Images)
















































